Abstract
Background and objective. Inotuzumab ozogamicin (InO) was approved for patients (pts) with relapsed/refractory (R/R) CD22-positive acute lymphoblastic leukemia (ALL) based on the results of INO-VATE trial (Kantarjian et al, 2016). There are scarce studies evaluating the results of InO therapy in real life in similar pts as those from the INO-VATE trial. Our objective was to analyze the outcomes of pts included in the compassionate program of InO in Spain (June 2013-April 2018) before definitive approval.
Patients and Methods. Inclusion criteria were age >18 yrs., CD22+ ALL, R/R resistant to ≥2 previous lines, Ph+ ALL resistant/intolerant to TKI, ECOG ≤2 or >2 if due to ALL, Bilirubin <1.5 ULN, AST & ALT <2.5 ULN, Creatinine ≤ 1.5 ULN. Exclusion criteria included mature B ALL, active CNS leukemia, chemotherapy in the two previous weeks, HSCT in the previous 6 months, grade ≥2 aGVHD or cGVHD, acute or chronic hepatitis B or C, HIV infection, VOD/SOS and antecedent chronic liver disease. Cycles of InO (0.8 mg/m 2 IV d1, and 0.5mg/m 2 IV on d8 and d15) were given every 21 days. Main outcomes: early death, CR/CRi, CR duration, PFS, OS and HSCT realization after InO.
Results. 34 pts were included in the trial, 21 males, median age 43 yrs (range 19-73), ECOG <2 22/26, WBC count 7.8 x10 9/L (0.3-388), pro B ALL 4/33, common 26/33, pre-B 3/33, Ph+ ALL 5/34 (15%), BM blast cells >50% 15/33 (45%). 25/34 (73%) of pts received >2 previous lines of therapy and 20 (59%) were previously transplanted. The duration of first CR remission before InO was <12 months in 16/33 pts (49%) and 16/34 pts were refractory to the last treatment before InO.
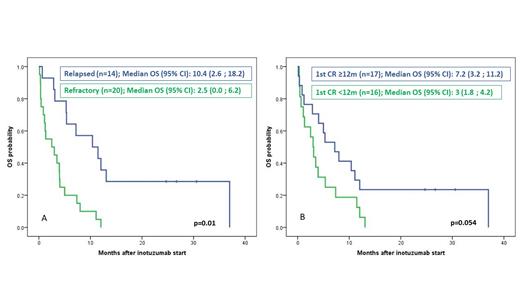
The median number of InO cycles was 2 (1-6). One pt withdrew the study before evaluation, 5 (15%) dead during therapy and 21 (64%) achieved CR/CRi. Ten pts (29%) were transplanted. With a median follow-up for alive patients after InO start of 26 months, the medians (95%CI) of DR, PFS and OS were 4.7 months (2.4-7.0), 3.5 (2.0-5.0) and 4.0 months (1.9-6.1), respectively. CR duration, PFS and OS were significantly shorter in refractory ALL (Figure 1A), pts with first CR (CR1) duration <12 months (Figure 1B) and in those without previous HSCT. The number of previous lines of therapy did not show impact on outcome.
The most frequent adverse events were hepatic (24%), infectious (18%), hematologic (15%) and gastrointestinal (9%). 3/10 transplanted patients showed grade 3-4 VOD/SOS. Grade 5 toxic events were hepatic (n=2), infection (n=2) and hemorrhage (n=1).
Conclusion. The results in this series of compassionate use of InO for R/R ALL before approval for clinical use were slightly inferior to that of the INO-VATE trial. However, patients form this series had poorer risk factors than those included in that trial. The frequency and type of AE were similar to that of observed in the INO-VATE trial.
Supported in part by grant 2017 SGR288 (GRC) Generalitat de Catalunya and "La Caixa" Foundation.
Figure 1. Overall survival according to ALL status at inotuzumab start (A) and to duration of first complete remission (B)
Ribera: AMGEN: Consultancy, Research Funding, Speakers Bureau; SHIRE: Consultancy, Speakers Bureau; ARIAD: Consultancy, Research Funding, Speakers Bureau; TAKEDA: Consultancy, Research Funding, Speakers Bureau; NOVARTIS: Consultancy, Speakers Bureau; Pfizer: Consultancy, Research Funding, Speakers Bureau. Hernández-Rivas: Celgene/BMS: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Novartis: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Pfizer: Honoraria, Membership on an entity's Board of Directors or advisory committees; Amgen: Honoraria, Membership on an entity's Board of Directors or advisory committees.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal